Prostatitis is a condition that affects countless men worldwide, yet it remains shrouded in silence and often misunderstood. The impact it can have on a man's physical and emotional well-being is significant, making it essential to raise awareness and promote early detection and effective treatment. In this blog post, we will delve into the world of prostatitis, shedding light on its causes, symptoms, diagnosis, and available treatment options. Let's break the silence and empower men to take control of their health.
Understanding Prostatitis
To begin our journey, it's important to understand what prostatitis is. Prostatitis refers to the inflammation of the prostate gland, a small walnut-sized organ located beneath the bladder. Acute bacterial prostatitis, chronic bacterial prostatitis, chronic prostatitis/chronic pelvic pain syndrome (CP/CPPS), and asymptomatic inflammatory prostatitis are the four kinds of prostatitis.
Each type presents with different symptoms and requires specific treatment approaches.

Understanding the cause
The exact causes of prostatitis are not fully understood, but some possible factors include:
- Bacterial infection: Bacteria from the urinary tract, the bowel, or the skin can enter the prostate through the urethra (the tube that carries urine and semen out of the body) or the blood. This can cause acute or chronic bacterial prostatitis. Some risk factors for bacterial infection include having a UTI, having an STI, having a catheter inserted into the bladder, having a prostate biopsy, or having anal sex.
- Non-bacterial inflammation: The prostate gland can become inflamed due to other reasons such as stress, nerve damage, muscle tension, immune system problems, allergies, or injury. This can cause chronic pelvic pain syndrome or asymptomatic inflammatory prostatitis. Some risk factors for non-bacterial inflammation include having a history of pelvic trauma, surgery, or infection, having an autoimmune disorder, having chronic pain conditions, or having psychological problems.
- Other factors: Some other factors that may contribute to prostatitis include genetics, hormones, age, diet, lifestyle, and environmental factors. However, more research is needed to understand how these factors affect the prostate and cause prostatitis.
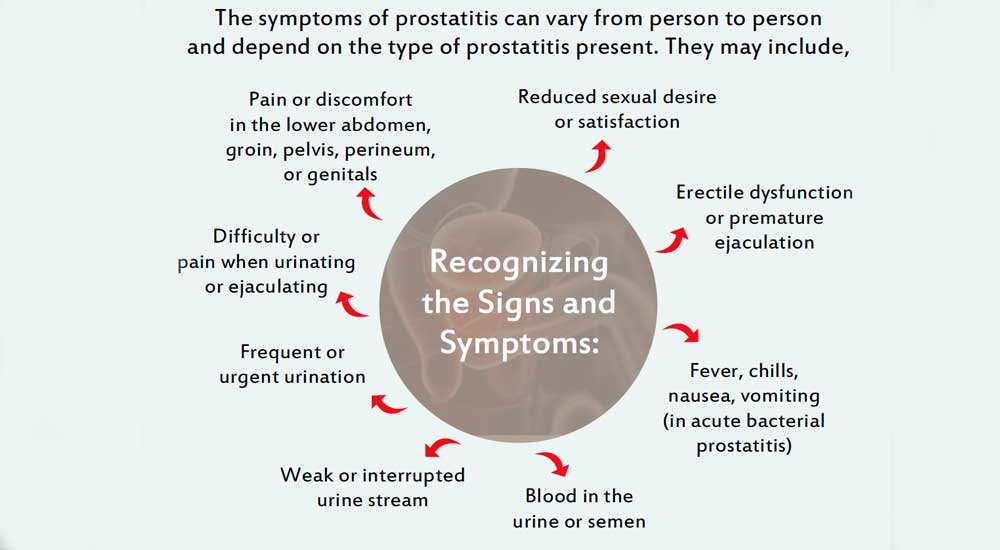
Some men with prostatitis may not have any symptoms at all or may have mild symptoms that come and go. However, some men may have severe symptoms that interfere with their daily activities and quality of life. By recognizing these signs early on, men can seek medical attention promptly, leading to better outcomes and improved quality of life.
Diagnosis: Seeking Clarity
Proper diagnosis is crucial for effective management of prostatitis. Urologists employ various methods, including a detailed medical history, physical examination, urine tests, prostate fluid analysis, and imaging studies, to accurately diagnose the condition. A thorough evaluation ensures the appropriate treatment plan can be tailored to the individual's specific needs.
Treatment and Prevention Options
The treatment of prostatitis is multifaceted and depends on the type and severity of the condition. Antibiotics are typically prescribed for bacterial prostatitis, while non-bacterial prostatitis often requires a combination of therapies such as pain management, alpha-blockers to relax the muscles, physical therapy, and lifestyle modifications.
Lifestyle changes may include:
Drinking plenty of water to flush out bacteria and toxins from the urinary tract.
Avoiding or limiting alcohol, caffeine, spicy or acidic foods, and artificial sweeteners, which can irritate the bladder and prostate.
Eating a balanced diet rich in fiber, fruits, vegetables, and omega-3 fatty acids, which can help reduce inflammation and support immune function.
Exercising regularly to improve blood circulation, reduce stress, and strengthen pelvic muscles.
Practicing good hygiene by washing your genitals and anus with mild soap and water, wiping from front to back after bowel movements, and urinating before and after sexual activity.
Using condoms or abstaining from sex if you have an active infection or an STI to prevent spreading bacteria to your partner or yourself.
Managing stress by using relaxation techniques such as deep breathing, meditation, yoga, or massage.
Seeking counseling if you have emotional or psychological problems related to prostatitis such as anxiety, depression, or low self-esteem.
Physical therapy
Your physical therapist can help you with exercises and techniques to improve your pelvic floor function and reduce pain. These may include:
Kegel exercises
strengthen the muscles that support the bladder, prostate, and urethra.
Biofeedback
helps you learn how to control your pelvic muscles and relax them when they are tense or spasming.
Trigger point therapy
releases tight knots of muscle tissue that cause pain and pressure in the pelvis.
Massage therapy
improves blood flow and reduces inflammation in the prostate and surrounding tissues.
Alternative therapy
Some men may find relief from prostatitis symptoms by using alternative therapies such as acupuncture, herbal remedies, homeopathy, or supplements. However, there is not enough scientific evidence to support the safety or effectiveness of these therapies for prostatitis. You should consult your Urologist before trying any alternative therapies and inform them of any products you are using. You should also be aware of the potential risks and interactions of these therapies with your medications or other treatments.
While prostatitis can be challenging to prevent entirely, by adopting these habits, men can promote overall prostate health and potentially minimize the impact of prostatitis.
Conclusion
Prostatitis is a condition that affects many men worldwide, yet it often remains hidden in the shadows. By breaking the silence and raising awareness, we can ensure that men receive the support, understanding, and effective treatment they need. Whether it's through early detection, accurate diagnosis, or exploring various treatment options, men should be encouraged to take charge of their health. Let's join hands to break the silence on prostatitis and empower men to live healthier, happier lives.
Dr. Amit Goel is a Consultant Laparoscopic/ Robotic Urologist & Renal Transplant Surgeon. He has over 15 years of experience in successfully treating complex urological diseases. His expertise includes diagnosing & treating Kidney stones, prostate enlargement, prostate cancer, kidney cancer, bladder cancer & incontinence, male infertility & erectile dysfunction.
