What is a Ureteroscopy?
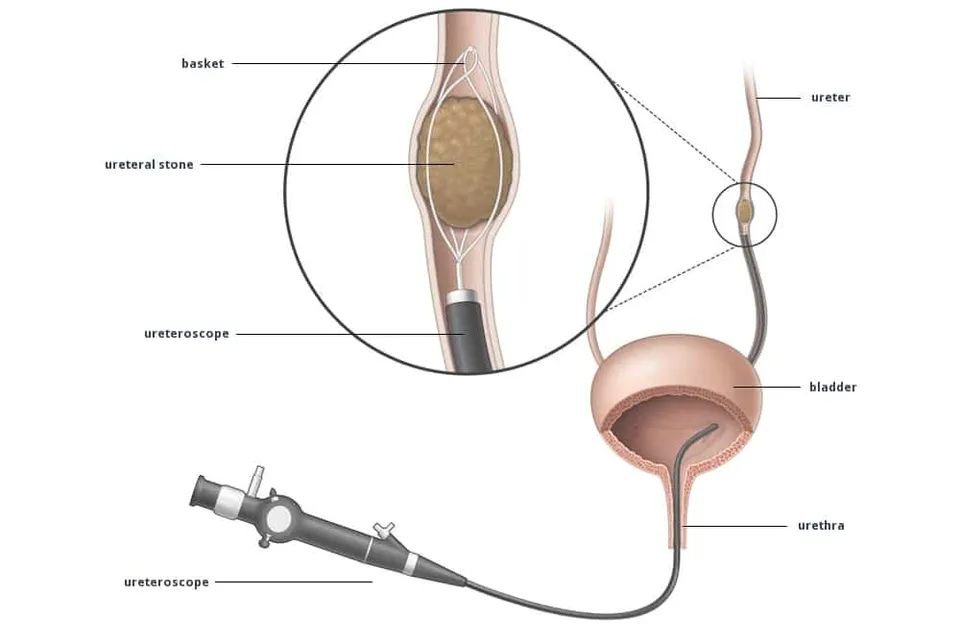
The urinary system is made up of the kidneys, ureter (narrow, muscular tube that connects your kidney to your bladder), bladder and urethra (tube that allows urine to pass through the bladder and out of the body). A ureteroscopy is a procedure that looks into the ureter and kidney. It involves inserting a special telescope, called a ureteroscope, into the urethra and then passing it through to the bladder and then on into the ureter and kidney. The operation is usually performed under generalanaesthetic. This means that you are asleepduring the procedure. Many a times, a spinal anaesthetic is used (where a needle is put in your back to numb you from the waist down) – your anaethetist will discuss the type of anaesthetic you need with you. The ureteroscope is about the thickness of a pencil and has a tiny camera on one end, so the doctor can view an image of your urinary system on a screen. It is usually used to treat kidney stones, but it is also used to help make a diagnosis for unexplained bleeding, assessment of some cancers in the ureter or kidney and to check if treatments have worked.
Why do I need a Ureteroscopy?
You have been advised to have a ureteroscopy to treat stones or to try to find the cause of your symptoms. Sometimes this will be clear from X-rays or tests of your blood or urine, but often the only way your doctor can be sure what is going on is to look inside your bladder and ureter. A ureteroscopy is commonly used to treat stone disease or cancers in the ureter and kidney.
It can help to diagnose the cause:
- abnormal cells in your urine
- blood in your urine (haematuria)
- pain (loin/back)
What are the risks associated with a Ureteroscopy?
There are risks associated with any operation. Your doctor will explain these risks to you before you sign the consent form. If you are unsure of anything, please make sure you ask your doctor. A ureteroscopy is usually performed with no problems whatsoever. However there is a possibility of:
- Discomfort – you may feel a stinging sensation when you urinate, but this should only last a day or two. Taking a normal pain-relieving tablet as prescribed may help. If the pain is severe and lasts for more than a couple of days, please contact us.
- Bleeding – you may have a small amount of bleeding as a result of the procedure - this is completely normal. Some patients do not have any bleeding at all, but some find their urine is slightly pink for a few days after this procedure. Drinking plenty of water (about three litres spaced out over 24 hours) can help to clear the urine. If your urine remains in pink after a few days, please contact us
- Infection – a urine infection can cause a fever and pain when you pass urine. The risk of this can be reduced by drinking plenty of water after the procedure. You will be given an injection of antibiotics when you have the anaesthetic.
- Stent insertion – you are likely to need a stent (a fine plastic tube) put in. The stent allows urine to drain from your kidney into your bladder when you have a blockage (such as a stone or growth) in your ureter (narrow, muscular tube that connects your kidney to your bladder)
- Unable to pass the telescope – in some patients the ureter (narrow, muscular tube that connects your kidney to your bladder) is too narrow to allow the telescope to pass. This occurs in approximately one in 20 cases. In this situation to avoid damaging the ureter, you will have a stent inserted and the procedure will be re-booked. The stent widens the ureter so usually the second procedure is more straight forward.
- Need for further procedures – sometimes the amount of stone will mean that a further procedure is required. Your doctor will discuss this with you.
- Ureteric stricture – a narrowing can form in the tube as a result of the procedure. This occurs in less than one in 100 cases.
- Ureteric injury – very rarely the ureter can get injured or damaged from the procedure. Great care is taken to avoid this. It is usually treated by inserting a ureteric stent.
Are there any alternatives?
A ureteroscopy is the only way to have a close enough look at the upper urinary system to diagnose certain ureter and kidney conditions. There are other options to fragment stones which your doctor will discuss with you.
What is a ureteric stent?
A ureteric stent is a thin plastic tube inserted into your kidney. It allows urine to drain from your kidney into your bladder when you have a blockage in your ureter (narrow, muscular tube that connects your kidney to your bladder). They are often inserted for people who have stones blocking their kidney and are usually required after a ureteroscopy to protect the tube where the telescope has been. In some patients the stent only needs to be left in for a few days.
What are the risks associated with a ureteric stent?
The stent may irritate your bladder causing you to feel a need to pass urine frequently.
- You may see blood in your urine on some occasions, this is made worse by physical activity such as going to the gym, walking, hoovering or carrying heavy bags. Even if your urine has a lot of blood in it, as long as you are passing urine this is fine. The blood in the urine may be cleared by drinking the recommended amount of daily fluids and will decrease as the days following the surgery pass.
- It is common to feel pain in your back (on the side of your body where the stent is) when passing urine. For most patients the symptoms are minor and can be tolerated.
- Occasionally the stent may develop a crystal coating on its surface and maybe difficult to remove. Usually this is not a significant problem but is the reason that we try not to leave the stent in for any longer than is needed.
- Very occasionally a stent may get displaced, usually slipping towards the bladder, and sometimes it may even fall out. This is very unusual. If this happens, please contact the hospital on the numbers listed at the end of this leaflet.
Having a stent, along with an underlying kidney problem, makes it more likely that you could develop a urinary tract infection (UTI). Some of the symptoms that you may experience should you get a UTI include a raised temperature, increased pain or discomfort in the kidney or bladder area, a burning sensation while passing urine and generally feeling unwell. UTI’s require treatment with antibiotics for few days.
Giving my consent (permission)
We want to involve you in decisions about your care and treatment. If you decide to go ahead, you will be asked to sign a consent form. This states that you agree to have the treatment and you understand what it involves.
How can I prepare for the procedure?
If you smoke, you may be asked to stop smoking, as this increases the risk of developing a chest infection or deep vein thrombosis (DVT). Smoking can also delay wound healing because it reduces the amount of oxygen that reaches the tissues in your body.
Medicines If you are taking any medication, these may need to be temporarily stopped or adjusted around the time of your surgery or treatment, you will be given information on how to do this at your Anaesthesia check up. Do not make any changes to your usual medicines and continue to take them unless you have been advised to do so. Please remember to bring them into hospital with you. If you are taking any medicines that thin your blood, such as antiplatelet medicines (for example aspirin or clopidogrel) or anticoagulant medicines (for examples warfarin or rivaroxaban), please tell your doctor or the nurse as you may need to stop them temporarily before your surgery. Also tell your doctor or nurse if you have diabetes as you may need to alter the dose of your diabetes medicines, as you will need to fast before the procedure. Please let us know if you are taking any regular medicines (including anything you buy yourself over the counter or any herbal or homeopathic medicines) and if you have any allergies to any medicines. Further information on stopping any medicines will be given to you when you come for pre-assessment.
What are the arrangements for coming to hospital?
You may be asked to attend a pre-admission appointment. This is to have blood tests and a physical examination, to make sure you are fit for the procedure. Your admission to hospital for your ureteroscopy will either be:
- The day before your operation or directly on the day of your operation. You will be told about the same in advance, at your pre-admission appointment.
- You will be told when to stop eating and drinking prior to the procedure, ideally 6-8 hrs of fasting ( no liquids or solids) is required before proposed surgery. If you continue to eat after this your surgery will be cancelled.
- You should have a shower or bath at home before arriving at the hospital .
What happens before the procedure?
Before your procedure you will be visited by the anaesthetist who will discuss the type of anaesthetic you will be given. Please remove all jewellery. If you have jewellery that cannot be removed, please let us know so that we can put tape on it. This is so that it does not interfere with our equipment. You may be taken to theatre on a trolley or you may walk to theatre, accompanied by a nurse.
What happens after the procedure?
Although you will be awake a minute or two after the procedure is finished, you are unlikely to remember anything until you are back in your bed. You may feel sick or be sick for up to 24 hours after the operation. This is an after effect of the anaesthetic. If this happens, we will give you some anti-sickness medication. You will be encouraged to start drinking as soon as possible, as long as you are not feeling sick. You may eat a light meal as soon as you feel able to once on the ward. You should be eating and drinking normally after two or three days. The anaesthetic may make you clumsy, slow and forgetful for about 24 hours. Although you may feel fine, your reasoning, reflexes, judgment, coordination and skill can be affected for 48 hours after your surgery. If you are discharged from the hospital less than 48 hours from your surgery, please rest when you get home and do not go to school or work on the day after your surgery. For 48 hours after your surgery for your safety please.
DO NOT:
- drive any vehicle, including a bicycle
- operate any machinery
- attempt to cook, use sharp utensils or pour hot or boiling liquids
- drink alcohol
- smoke
- take sleeping tablets
- make any important decisions or sign any contracts.
How long should the stent stay in?
The length of time a stent needs to stay in is different for every patient and your doctor will discuss this with you. After a ureteroscopy it is commonly left in for between 1 week and 3 weeks. They can occasionally be left for much longer if needed. It is very important that the stent is removed at the correct time. If you are concerned that you have not had your stent removed, please contact us immediately.